Case managers face unique challenges when trying to match patients with the right dialysis setting. Dialyze Direct offers several tools and resources to help streamline the process:
Trach/Vent patients: Use the filters on our Location Finder to quickly identify SNF facilities that can accept these referrals.
Infection Control Needs: For patients with Candida Auris or other infection control concerns, our Intake Coordinators can help identify SNFs equipped to accept these cases. Contact our Intake Coordinators for more information.
Open Chairs: Stay updated on facility availability. Dialyze Direct can provide weekly emails listing open chairs in each state. To subscribe, email us! at Info@dialyzedirect.com
Dialyze Direct is now offering home dialysis services for eligible patients, providing more options for case managers who work to place individuals in the most appropriate setting.
Our home program is available to patients who meet criteria based on location, insurance coverage, and comorbidities. This expansion builds on our existing model in skilled nursing facilities, giving case managers another pathway to help patients receive high-quality, coordinated dialysis care without unnecessary delays.
To check availability in your area or start a referral, visit our home dialysis referral page
We’re committed to making placements faster and smoother—whether for SNF residents or patients who can safely receive treatment at home.
Chronic kidney disease (CKD) is a growing health concern, affecting 1 in 7 adults in the United States, nearly 37 million people, according to the Centers for Disease Control and Prevention (CDC). Alarmingly, 90% of those with CKD are unaware they have it until the disease has progressed to more severe stages (National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)).
Often called a “silent disease,” CKD develops gradually, with no noticeable symptoms in the early stages. By the time most people receive a diagnosis, significant kidney damage has already occurred, increasing their risk of kidney failure, heart disease, stroke, and even death.
The kidneys play a vital role in filtering toxins and excess fluids from the blood, regulating blood pressure, producing red blood cells, and maintaining electrolyte balance. When kidney function declines, these essential processes are disrupted, leading to severe health complications. In fact, CKD and heart disease are closely linked, as reduced kidney function increases the risk of cardiovascular problems.
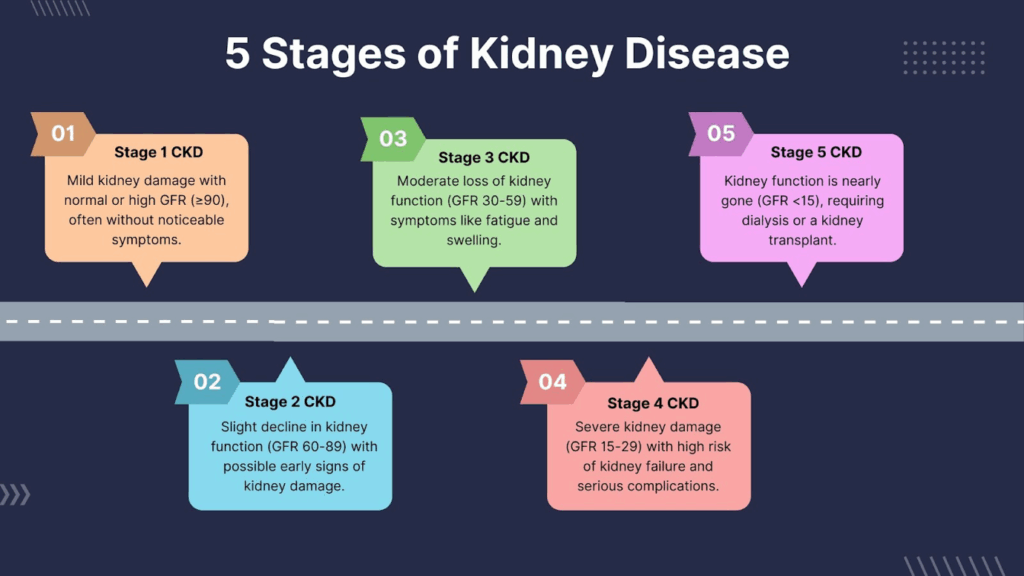
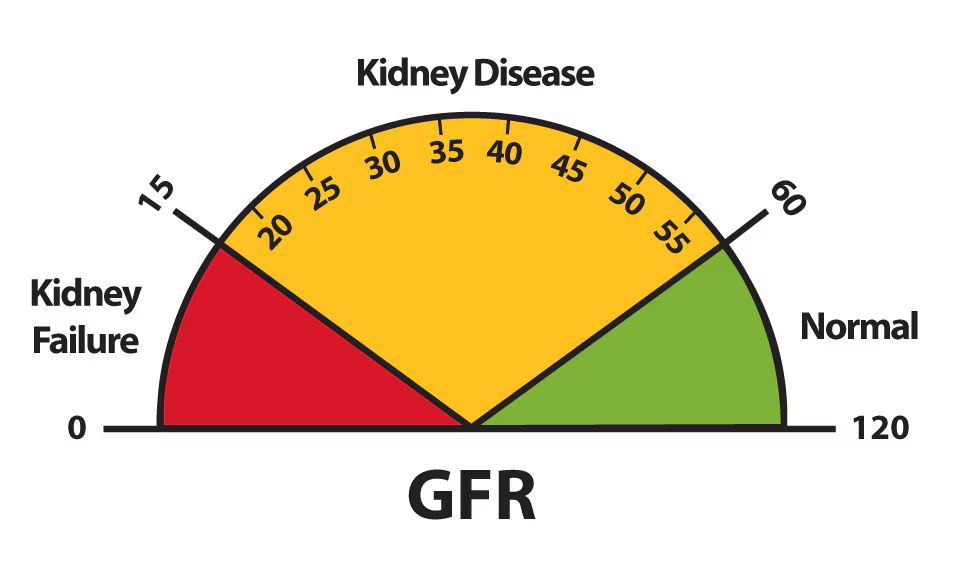
The stages of CKD are determined by the glomerular filtration rate (GFR) which is calculated using serum creatinine levels, and is a measure of how well the kidneys filter waste.
GFR: 90 or above (kidneys function normally but show damage signs).
Possible Signs:
Fact: At this stage, lifestyle changes and/or other interventions may mitigate further kidney damage.
Management:
Control of risk factors. The detailed management depends on the underlying cause. For example, control of hypertension or diabetes can help. Appropriate dietary interventions (lowering dietary sodium, sweets or protein) may also be appropriate. Regular kidney function monitoring should be initiated.
GFR: 60-89
Symptoms:
Mild changes in urine output or urine character (e.g., foamy urine may occur with more significant urinary protein losses), or mild fluid retention causing lower extremity swelling (edema) may also be present.
Fact: People with high blood pressure or uncontrolled diabetes are at higher risk of CKD progression.
Management:
In addition to hypertension and diabetes management, regular kidney function tests must be carefully tracked. Avoid NSAIDs (like ibuprofen), which can accelerate kidney damage.
GFR: 30-59
Symptoms:
Fatigue and weakness can manifest due to the development of advanced CKD-related anemia. More extensive swelling of the feet (and sometimes hands and face) may be associated with more fluid retention.
Complications of CKD: Increased risk of heart and vascular disease. At this stage of kidney disease, abnormalities of calcium, phosphorus, and bone metabolism begin to manifest.
Fact: At Stage 3, 1 in 3 people with CKD may develop end-stage kidney disease (ESKD) without proper management.
Management:
Medications to control blood pressure, blood sugar, and phosphorus levels may be indicated. Reduced protein intake may also be indicated in some circumstances to lessen the burden on the kidneys.
GFR: 15-29
Symptoms:
Fact: More than 50% of people with Stage 4 CKD will develop kidney failure within five years.
Management:
Rule out any superimposed kidney obstruction with imaging studies, even if it was ruled out at an earlier stage of kidney disease. Begin discussing dialysis and/or kidney transplant options with your kidney specialist. Carefully monitor and manage anemia and electrolyte imbalances.
GFR: Below 15 (kidney function is at a critically low level).
Symptoms:
Severe fatigue, weakness, confusion due to toxin buildup and anemia. Shortness of breath due to fluid in the lungs. Significant swelling (legs, around the eyes, and abdomen).
Treatment Options:
Dialysis (hemodialysis or peritoneal dialysis) to filter toxins from the blood. Kidney transplantation (if appropriate) offers the best long-term survival outcome. Home dialysis is an option for many patients, offering flexibility, improved quality of life and superior medical outcomes. Learn more about home dialysis here.
Albuminuria is a key indicator of kidney disease, referring to the presence of albumin (a type of protein) in the urine. Healthy kidneys typically prevent normal blood protein from leaking into the urine, but when kidney function declines, significant protein in the urine signals kidney damage. Measuring albuminuria helps assess the severity of chronic kidney disease (CKD) and predict the risk of progression to kidney failure.
The National Kidney Foundation classifies albuminuria into three stages based on the albumin-to-creatinine ratio (ACR) in milligrams (mg) albumin per gram (g) creatinine):
A1 (Normal to Mild Albuminuria)
ACR: Less than 30 mg/g
This level is considered normal or mildly increased. It typically does not indicate significant kidney damage. However, people with diabetes, high blood pressure, or other CKD risk factors should monitor their kidney health closely.
A2 (Moderate Albuminuria, formerly known as Microalbuminuria)
ACR: 30–300 mg/g
A moderate increase in albumin levels suggests early kidney damage. At this stage, CKD may still be reversible with lifestyle changes and medication to control blood pressure, diabetes, and other contributing factors.
A3 (Severe Albuminuria, formerly known as Macroalbuminuria)
ACR: More than 300 mg/g
A high level of albumin in the urine indicates significant kidney damage. This stage is associated with a higher risk of CKD progression, cardiovascular disease, and end-stage kidney disease (ESKD), requiring dialysis or a kidney transplant.
A simple urine albumin-to-creatinine ratio (uACR) test can detect albuminuria. The National Kidney Foundation recommends regular testing for individuals at high risk, including those with diabetes, high blood pressure, or a family history of kidney disease.
Understanding albuminuria stages can help people with CKD take proactive steps to preserve kidney function and prevent the progression of kidney failure.
CKD can develop due to various underlying conditions, with diabetes and high blood pressure being the leading causes.
African American, Hispanic, Asian, and Native American populations have a higher genetic predisposition, but proteinuria can also occur in individuals of any heritage.
At Dialyze Direct, we understand how overwhelming a CKD diagnosis can feel. That’s why we provide personalized, more frequent home hemodialysis treatments inside SNFs or within a patient’s home. Our approach is designed to be gentler on the body, easier to fit into daily life, and to provide superior medical outcomes.
If you’re a patient, caregiver, or healthcare provider, contact Dialyze Direct today to learn how we can help support better outcomes for people living with advanced kidney disease.
Phone: (732) 732-0052
Web Address: https://www.dialyzedirect.com/contact/
Life expectancy varies and is influenced by the underlying medical conditions. However, with proper management, many people with stage 3 CKD can live for decades without progressing to kidney failure.
The five stages of CKD range from mild kidney damage (Stage 1) to end-stage kidney disease (Stage 5), classified by glomerular filtration rate (GFR) levels.
It is recommended to see a nephrologist by Stage 3 CKD to monitor kidney function and slow disease progression. Often a nephrologist is seen at an even earlier stage of kidney disease.
While CKD is generally not reversible, lifestyle changes, medication, and proper disease management can slow or halt its progression.

Dr. Allen Kaufman is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct, with over four decades of experience in Nephrology. He began his career in 1980 and has held leadership roles including Chief of Nephrology & Hypertension at Beth Israel Medical Center (1998–2004), Chief of Dialysis at the Bronx VA Medical Center (1982–1990), and Chief of the Yorkville Dialysis Unit at Beth Israel and the Renal Research Institute (1990–2000). Dr. Kaufman has authored over 100 scientific publications and served as Principal or Co-Investigator on numerous NIH-funded research studies. A Fellow of the American College of Physicians, he is board-certified in Nephrology and Internal Medicine. He earned his medical degree from the University of Rochester and completed training at the Hospital of the University of Pennsylvania and Mount Sinai in New York. Dr. Kaufman is widely recognized with multiple “Best Doctor” and “Patients’ Choice” awards.
Kidney disease is often referred to as a “silent killer” because it can develop with little to no symptoms in its early stages. However, recognizing the warning signs early can help you take proactive steps to protect your kidney health and prevent further complications. Here’s what you need to know about the early signs of kidney disease and when to seek medical attention.
The kidneys play a vital role in filtering waste products and excess fluids from the blood, regulating blood pressure and kidney function, and balancing essential nutrients in the body. When they begin to lose function, waste can build up, leading to serious health complications, including chronic kidney disease (CKD), acute kidney injuries, and kidney failure.
According to the Centers for Disease Control and Prevention (CDC), millions of Americans suffer from kidney disease, yet many are unaware they have it. Common causes of chronic kidney disease include diabetes, high blood pressure, autoimmune disease, and polycystic kidney disease.
Many people with chronic kidney disease may not experience symptoms until significant kidney damage has occurred.
However, some early warning signs to watch for include:
The kidneys filter waste from the blood to produce urine. Any noticeable change in urination, such as:
A urine test can help diagnose kidney disease and detect abnormalities at an early stage.
When kidney function declines, waste products accumulate in the blood, leading to a condition known as uremia. This can cause extreme tiredness, weakness, and a lack of concentration. Additionally, kidney disease can lead to anemia due to a decrease in red blood cells, further contributing to fatigue.
The kidneys regulate fluid balance in the body. When they fail to function properly, fluid builds up, causing swelling in the legs, feet, hands, and face. This is a sign of fluid retention, often linked to high blood pressure and kidney damage.

Excess fluid from kidney disease can accumulate in the lungs, leading to breathing difficulties. Low red blood cell levels can also result in reduced oxygen delivery, worsening symptoms of shortness of breath.
Kidneys remove toxins from the body. When kidney function is compromised, waste products build up in the blood, causing severe itching, rashes, and dry skin.

A buildup of toxins due to declining kidney function can result in nausea, vomiting, and loss of appetite. Many people with kidney disease experience an aversion to certain foods, leading to unintended weight loss.
The kidneys help regulate blood pressure, and their decline can contribute to hypertension. In turn, high blood pressure is a leading cause of kidney disease, creating a vicious cycle. Uncontrolled high blood pressure increases the risk of kidney failure and blood vessel damage.
If you experience any of these symptoms, it is essential to consult a kidney specialist. Early detection through medical tests can help diagnose kidney disease and prevent further damage.
For individuals with end-stage renal disease (ESRD) or end-stage kidney disease, treatment includes dialysis or a kidney transplant. Dialysis helps remove excess fluids and waste from the body, replacing kidney function. Some people may require a kidney transplant to survive, as this can offer a long-term solution to kidney failure.
Many patients opt for home dialysis, which provides flexibility and greater independence in managing kidney disease from the comfort of their homes.
Kidney disease can be prevented or slowed with early detection and proper treatment. If you’re at risk due to diabetes, high blood pressure, or a family history of kidney disease, taking proactive steps can help reduce the risk of developing kidney failure.
Key Takeaways:
Recognizing the symptoms of chronic kidney disease early and seeking timely intervention can make a huge difference in your kidney health and overall well-being. To learn more about treatment options, including home dialysis, visit Dialyze Direct.
References and links
Information contained in this blog is for informational or educational purposes only and does not substitute professional medical advice or consultations with healthcare professionals. The content is not meant to be complete or exhaustive or to apply to any specific individual’s medical condition. Always refer to the personalized information given to you by your doctor or contact us directly.
Allen Kaufman MD has been practicing Nephrology since 1980. He is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct since its inception in 2016. In New York City he served as the Chief of Dialysis at the Bronx Veterans Administration Medical Center from 1982-1990, the Chief of Beth Israel Medical Center’s Yorkville Dialysis Unit from 1990-2000 and, subsequently, the Chief of the Division of Nephrology & Hypertension from 1998-2004.

Dr. Allen Kaufman is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct, with over four decades of experience in Nephrology. He began his career in 1980 and has held leadership roles including Chief of Nephrology & Hypertension at Beth Israel Medical Center (1998–2004), Chief of Dialysis at the Bronx VA Medical Center (1982–1990), and Chief of the Yorkville Dialysis Unit at Beth Israel and the Renal Research Institute (1990–2000). Dr. Kaufman has authored over 100 scientific publications and served as Principal or Co-Investigator on numerous NIH-funded research studies. A Fellow of the American College of Physicians, he is board-certified in Nephrology and Internal Medicine. He earned his medical degree from the University of Rochester and completed training at the Hospital of the University of Pennsylvania and Mount Sinai in New York. Dr. Kaufman is widely recognized with multiple “Best Doctor” and “Patients’ Choice” awards.
Chronic kidney disease (CKD) often progresses quietly, many people don’t realize there’s a problem until it’s fairly advanced. That’s why it’s important to understand what signs to look for and when to seek medical attention. CKD can develop slowly over months or years, and the symptoms can be vague at first. But paying attention to your body, especially if you’re in a high-risk group, can make a big difference in catching the disease early.
“Because kidney disease doesn’t usually cause pain or obvious symptoms in the early stages, many patients don’t know they’re at risk until significant damage has occurred,” says Dr. Allen Kaufman, MD , Chief Medical Officer, Senior VP Clinical & Scientific Affairs with Dialyze Direct. “If you notice any unusual symptoms, especially if you have diabetes, high blood pressure, or a family history of kidney disease, don’t ignore them. Ask for a kidney function test.”
In the early stages, symptoms may be mild or even nonexistent. If there are signs, they can be easy to brush off:
These symptoms are nonspecific and often mistaken for other conditions, but they can be early indicators of kidney stress.
As CKD progresses, signs become more noticeable. These might include:

None of these symptoms are exclusive to CKD, but when they show up, they should prompt further evaluation.
It’s a good idea to get checked if you notice:
If you have a family history of kidney disease, it’s important to get screened, even if you feel fine.
Certain people are more likely to develop CKD, even without symptoms. If you fall into any of these categories, talk to your doctor about routine kidney function tests:
Kidney disease is often manageable, especially when caught early. Regular screening through blood and urine tests can detect problems before symptoms develop. If you’re concerned about CKD or fall into a high-risk group, don’t wait for symptoms to appear.
At Dialyze Direct, we specialize in providing on-site dialysis in skilled nursing facilities and now within our patients’ homes, helping patients receive care in a more comfortable and convenient setting. Learn more about how our model works or explore our locations to see where we offer services near you.For more information about kidney disease, symptoms, and prevention, visit the National Kidney Foundation.
Information contained in this blog is for informational or educational purposes only and does not substitute professional medical advice or consultations with healthcare professionals. The content is not meant to be complete or exhaustive or to apply to any specific individual’s medical condition. Always refer to the personalized information given to you by your doctor or contact us directly.
Review:
This content has been reviewed by Dr. Allen Kaufman, MD , Chief Medical Officer, Senior VP Clinical & Scientific Affairs with Dialyze Direct, to ensure clinical accuracy and reliability.

Dr. Allen Kaufman is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct, with over four decades of experience in Nephrology. He began his career in 1980 and has held leadership roles including Chief of Nephrology & Hypertension at Beth Israel Medical Center (1998–2004), Chief of Dialysis at the Bronx VA Medical Center (1982–1990), and Chief of the Yorkville Dialysis Unit at Beth Israel and the Renal Research Institute (1990–2000). Dr. Kaufman has authored over 100 scientific publications and served as Principal or Co-Investigator on numerous NIH-funded research studies. A Fellow of the American College of Physicians, he is board-certified in Nephrology and Internal Medicine. He earned his medical degree from the University of Rochester and completed training at the Hospital of the University of Pennsylvania and Mount Sinai in New York. Dr. Kaufman is widely recognized with multiple “Best Doctor” and “Patients’ Choice” awards.
More frequent dialysis provides a slower rate of dialytic fluid removal and stabilizes intradialytic hemodynamics. In those patients with acute kidney injury (AKI) who require dialysis therapy, this gentler dialysis model of care may enhance the chances of kidney recovery and liberation from dialytic care.
Key points on why this approach may lead to better outcomes for AKI patients.
Improved Clinical Outcomes for AKI Patients
More frequent dialysis sessions improve the way toxins and excess fluids are removed, help maintain stable electrolyte levels, and enhance hemodynamic stability. This model of care can be especially beneficial for patients with acute kidney injury (AKI), as it mitigates complications like pulmonary edema, arrhythmias, and hypotension—ultimately supporting faster recovery and protecting vital organs and permits on-site management of patients with higher levels of medical complexity and more comorbid conditions
Reduced Risk of Complications
Dialysis removes fluid more gently (1) and can lower the risk of cardiovascular events, and other complications associated with more crude methods of fluid removal.
Reduced Hospitalizations and Continuity of Care
When AKI patients receive dialysis onsite at a SNF, any health events or complications can be managed immediately by the facility’s clinical team, avoiding unnecessary hospital transfers. Instead of being sent to the hospital, patients are returned to their rooms for prompt care and monitoring, supporting faster stabilization and continuity of treatment.
More Time for Rehab
Onsite dialysis with more frequent dialysis eliminates the need for time-consuming transportation to offsite clinics, reduces post-dialysis recovery time 2, and frees up valuable hours in the day. This results in patients spending up to 70% more time participating in rehab, which can accelerate recovery and improve overall outcomes, including moving up the date of discharge home.
At Dialyze Direct, where home-based and SNF (skilled nursing facility) dialysis models prioritize patient-centric care, a more frequent dialysis schedule aligns well with improving outcomes for AKI patients, particularly those with comorbidities.
On-site More Frequent Dialysis May Hasten Return Home for Nursing Home End-Stage Renal Disease Patients. Kidney 360. 2024; 10-34067.
Post-dialysis recovery time in ESRD patients receiving more frequent hemodialysis in skilled nursing facilities. Hemodialysis International. 2022;26(3):424-434.
Medically Reviewed: This content has been reviewed for clinical accuracy and reliability by Dr. Allen Kaufman, Chief Medical Officer at Dialyze Direct.

Dr. Allen Kaufman is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct, with over four decades of experience in Nephrology. He began his career in 1980 and has held leadership roles including Chief of Nephrology & Hypertension at Beth Israel Medical Center (1998–2004), Chief of Dialysis at the Bronx VA Medical Center (1982–1990), and Chief of the Yorkville Dialysis Unit at Beth Israel and the Renal Research Institute (1990–2000). Dr. Kaufman has authored over 100 scientific publications and served as Principal or Co-Investigator on numerous NIH-funded research studies. A Fellow of the American College of Physicians, he is board-certified in Nephrology and Internal Medicine. He earned his medical degree from the University of Rochester and completed training at the Hospital of the University of Pennsylvania and Mount Sinai in New York. Dr. Kaufman is widely recognized with multiple “Best Doctor” and “Patients’ Choice” awards.
Did you know that chronic kidney disease (CKD) is a growing concern, affecting approximately 37 million adults in the U.S., according to the Centers for Disease Control and Prevention (CDC). The alarming fact is that 90% of people with CKD don’t know they have it until it progresses to more severe stages.
That’s why kidney function tests, including the estimated glomerular filtration rate (eGFR) test and creatinine blood test, are crucial in detecting problems early and managing CKD effectively.
If CKD progresses, treatment options like dialysis or a kidney transplant may become necessary. Many patients now prefer home dialysis as a more flexible and convenient alternative to in-center treatments, allowing for greater independence and improved quality of life. Learn more about home dialysis here.
The estimated glomerular filtration rate (eGFR) is a key indicator of how well your kidneys filter blood. It is calculated based on creatinine levels, age, sex, and race and helps determine the stage of kidney disease.
| eGFR Level (mL/min) | Kidney Function |
| 90+ | Normal kidney function |
| 60–89 | Mildly decreased function (Early signs of CKD) |
| 30–59 | Moderate CKD (Stage 3) |
| 15–29 | Severe CKD (Stage 4) |
| Less than 15 | Kidney failure (Dialysis required) |
A low eGFR may indicate kidney damage, requiring additional tests to confirm results.
Kidney disease often progresses silently, making early detection crucial. One of the best ways to assess kidney function is by using an eGFR calculator, which estimates how well your kidneys are filtering waste from your blood.
An eGFR (Estimated Glomerular Filtration Rate) Calculator is a simple yet effective tool that helps estimate kidney function using key factors like:
The eGFR result helps determine chronic kidney disease (CKD) stages and guides doctors in treatment planning.
The most commonly used CKD-EPI equation estimates eGFR based on the following formula:
| eGFR Level (mL/min) | Kidney Function |
| 90+ | Normal kidney function |
| 60–89 | Mildly decreased function (Early signs of CKD) |
| 30–59 | Moderate CKD (Stage 3) |
| 15–29 | Severe CKD (Stage 4) |
| Less than 15 | Kidney failure (Dialysis required) |
A low eGFR may indicate kidney damage, requiring additional tests like creatinine blood tests and urine albumin tests to confirm kidney disease.
Take control of your kidney health today. Use This eGFR Calculator to quickly estimate your kidney function and understand your results.
A creatinine blood test measures the amount of creatinine in your blood, a waste product from the normal breakdown of muscle tissue. High creatinine levels may mean you have kidney disease, as your kidneys may not be working properly.
Normal creatinine levels:
Since creatinine is a waste product, the body normally filters it out through urine. If levels are high, it may indicate kidney filtration problems.
This blood test measures the amount of waste product in your blood called urea nitrogen. High BUN levels may suggest kidney disease, dehydration, or high protein intake.
The UACR test checks for albumin in your urine, which may be an early sign of kidney disease.
A urine test is often used alongside an eGFR test to confirm the cause of your kidney disease.
This test measures how effectively your kidneys remove creatinine from your blood over a 24-hour period. It provides further insights into glomerular filtration rate (GFR) and kidney function.
If other test results suggest kidney disease, a kidney biopsy may be necessary. This involves taking a small sample of kidney tissue to identify the cause of your kidney disease.
CKD is categorized into five stages based on eGFR levels:
| Stage | eGFR Level | What Happens? |
| Stage 1 | 90+ | Kidney damage, but normal function |
| Stage 2 | 60-89 | Mild decline in kidney function |
| Stage 3 | 30-59 | Moderate CKD; possible symptoms |
| Stage 4 | 15-29 | Severe CKD; preparing for dialysis or a kidney transplant |
| Stage 5 | <15 | Kidney failure; treatment required |
Knowing your kidney numbers (eGFR and creatinine levels) helps monitor CKD progression.
Kidney disease often develops slowly and silently, with symptoms appearing in later stages. Identifying risk factors early can help prevent or delay kidney damage. Several conditions and lifestyle choices increase the likelihood of developing chronic kidney disease (CKD) or kidney failure.
Warning Signs of Kidney Disease:
If your eGFR is less than 60 or your creatinine blood test shows abnormal results, consult a kidney specialist immediately.
When kidney function declines to the point of failure, hemodialysis is the most effective and widely recommended treatment. This process removes waste, excess fluids, and toxins from the blood, performing the vital filtration work that failing kidneys can no longer manage.
Many patients are now choosing home hemodialysis for its added convenience and effectiveness.
Worried about the cost of dialysis? Many insurance plans cover dialysis treatments. Learn more about dialysis insurance coverage here.
Peritoneal dialysis (PD) is another option where a special fluid is introduced into the abdomen to remove toxins and excess fluids. While PD offers more flexibility and does not require a machine during the treatment, it may not be suitable for everyone due to:
For most individuals with chronic kidney disease, hemodialysis remains the safer, more effective, and more widely supported treatment option. Consulting with a nephrologist can help determine the best approach for managing kidney failure effectively.
Kidney disease can progress silently, but early detection is key. If you’re at risk due to diabetes, high blood pressure, or family history, regular testing can help catch problems early.
For those with kidney failure, hemodialysis is a reliable and effective treatment that helps maintain quality of life. Many patients are now choosing home dialysis for its added flexibility and comfort.
Worried about the cost of dialysis? Many insurance plans cover dialysis treatments.
Learn more about dialysis insurance coverage here
Taking proactive steps to monitor your health, staying active, and following a kidney-friendly diet can make a big difference.
Driven, adaptable, and passionate about personal and professional growth, I bring a unique blend of creativity, problem-solving, and commitment to everything I do. With a strong background in [insert field or industry], I thrive in fast-paced environments where innovation and collaboration are key. I take pride in building strong relationships, delivering high-quality results, and constantly seeking new ways to learn and improve.
Throughout my journey, I’ve embraced challenges as opportunities for growth and continually pushed myself to exceed expectations. I’m highly organized, detail-oriented, and never shy away from taking initiative. Whether working independently or as part of a team, I believe in maintaining a positive attitude and a strong work ethic.
Starting January 1, 2025, Dialyze Direct is thrilled to announce a groundbreaking change in our admission policy for Medicare patients. Previously, an End-Stage Renal Disease (ESRD) diagnosis was required to admit patients to our home dialysis program. However, with the new regulations, we can now accept all Medicare patients with Acute Kidney Injury (AKI) , regardless of the underlying cause.
This significant policy shift opens up new opportunities for Medicare patients who need dialysis care. By removing the ESRD diagnosis requirement, we can now provide our specialized home dialysis services to a broader range of patients. This change is particularly beneficial for those with Acute Kidney Injury (AKI).
One of the most exciting aspects of this change is the ability to offer home dialysis in our partnered Skilled Nursing Facilities (SNFs) {locations}. These facilities provide a comprehensive range of rehabilitative services, ensuring that patients receive holistic care tailored to their individual needs. Here are some key benefits:
At Dialyze Direct, our mission is to enhance the quality of life for our patients. By expanding access to our home dialysis program, we are taking a significant step toward achieving this goal. Patients will benefit from the flexibility and comfort of home dialysis, combined with the comprehensive support available in SNFs.
We are excited about the positive impact this change will have on our patients and their families. As we move forward, Dialyze Direct remains committed to providing the highest quality of care and support to all our patients. We look forward to welcoming more Medicare patients into our home dialysis program and helping them achieve better health outcomes.
For more information about our home dialysis program and the services we offer, please visit our website or contact us directly. Together, we can make a difference in the lives of those living with kidney failure.
For more information on the Dialyze Direct difference and SNF onsite more frequent dialysis (MFD), email hello@dialyzedirect.com.
Patients with end-stage kidney disease (ESKD) who require dialysis often find themselves caught in what feels like an endless cycle of long dialysis sessions followed by lengthy recovery periods. Traditional dialysis, which requires travel to a dialysis clinic three times per week for treatment, has a high impact on quality of life for these patients.
In contrast, onsite dialysis, performed at the skilled nursing facility (SNF) where a patient resides, allows for more frequent, shorter dialysis sessions (pursuant to a physician’s order). These patients no longer have to endure lengthy transportation to and from their treatments, and even better, have a faster recovery allowing them to focus on rehabilitation or other activities between sessions.
Residents of skilled nursing facilities who also need dialysis are often older, frail, and have multiple comorbidities. Alongside dialysis, they typically have rehabilitation activities scheduled. Traditional dialysis can take up to six hours or more to complete (including transportation to/from a dialysis center). Plus, with up to 21 hours of post-treatment recovery time, it is easy to see how a Monday-Wednesday-Friday routine could interfere with rehabilitation and daily life for these patients.
Consider the example of Gladys, a 72-year-old skilled nursing facility (SNF) resident who was discharged to the SNF from the hospital after a fall. Gladys needs physical therapy due to a hip injury sustained in her fall, and dialysis due to her End Stage Kidney Disease (ESKD). She also has a history of congestive heart failure. This is a typical day for Gladys, who is scheduled for traditional dialysis at an off-site treatment center:
Dialyze Direct partners with a SNF facilities to offer onsite, patient-centric dialysis in treatment “dens” to patients that exhibit co-morbidities that are deemed medically reasonable and necessary to receive more frequent dialysis (MFD). Their overall plan of care is supported and supervised by a team of experts including specially trained nurses.
John, a 75-year-old grandfather of five, has recently been transferred to a skilled nursing facility following a hospital stay due to pneumonia. He’s deconditioned from his illness, requires rehabilitation services, and has a history of ESKD. A typical day for him is as follows:
As illustrated by these patient stories, there is a significant difference in outcomes between traditional dialysis and MFD. Research has shown that traditional dialysis commonly results in hospital admissions on the day of treatment and that rates of sudden cardiac death following this type of dialysis are highest on Mondays.
In contrast, MFD is gentler, resulting in fewer complications. In fact, Dialyze Direct has seen 65% fewer dialysis-related hospitalizations and a 94% reduction in vascular infections in patients receiving this model of care. In addition, MFD results in faster post-treatment recovery times. 92% of patients report recovery to baseline within 2 hours of treatment. Lastly, onsite SNF dialysis significantly reduces patient risk of infection, including COVID-19, by eliminating exposure at the offsite dialysis center.
Alongside these benefits to SNF patients with ESKD, there is a benefit for other key stakeholders as well. Transportation costs are reduced by 100% since patients do not need to leave the SNF for dialysis, and better patient outcomes drive high success rates with complex ESKD patients, a benefit for SNFs participating in patient-driven payment models (PDPM).
This patient population is projected to grow; currently, the rate of increase for ESKD is roughly 21,000 additional patients each year in the U.S., with Medicare devoting $80 billion a year to treating patients with chronic kidney disease.
For all reasons outlined above, MFD holds significant potential as a driver of cost-effective, improved long-term outcomes for patients. These include fewer complications, lower hospitalization rates, increased access to rehabilitation services, and quality-of-life enhancements. Because these positive results have potential to extend beyond the SNF, they merit continued investment in this modality of care.
For more information on the Dialyze Direct difference and SNF onsite more frequent dialysis (MFD), email hello@dialyzedirect.com.

Alice Hellebrand, DNP, RN, CNN has been with Dialyze Direct since its inception in 2015 and is responsible for overseeing the design and implementation of patient care delivery, clinical staff education, and clinical quality improvement. She has authored many journal publications and her expertise has been sought as a presenter nationally and internationally at nephrology, dialysis, and skilled nursing conferences. Her continued dedication to the Dialyze Direct model of dialysis care gives her unique insights into this pioneering approach to treatment.


Conventional hemodialysis (HD) is known to cause prolonged, debilitating post-dialysis symptoms. HD’s long recovery time seriously impacts the health and quality of life of end-stage kidney disease (ESKD) patients who reside in skilled nursing facilities (SNFs). Dialyze Direct hypothesized that more frequent dialysis (MFD) results in shorter recovery times for HD patients and better patient outcomes and sought to illustrate this with a study.
Patients age 65 or older with ESKD who receive dialysis total 52% of dialysis patients in the U.S. each year.1 Many of these patients reside in SNFs for a period of their treatment. Conventional dialysis involves transportation from the SNF to a dialysis center for treatment, three days per week.
Following these dialysis treatments, which occupy most of the day with transportation included, patients experience a long post-dialysis recovery time. Multiple studies have noted this can exceed four hours.2,3 In one study, 10% of patients reported even greater than twelve hours’ recovery time.4
Common dialysis symptoms include fatigue or feeling “washed out,” cramping, headaches, nausea, and low blood pressure.5 These adverse effects can cause patients to skip treatment or shorten sessions.6
Longer recovery times are associated with poorer quality of life and increased hospitalization and mortality risk.7 For patients who receive rehabilitation services at the SNF, this time away for dialysis and recovery may also interrupt their rehabilitation.
MFD is becoming more common in skilled nursing facilities (SNFs), provided that the patient exhibits co-morbidities that are medically reasonable and necessary to receive MFD. Dialyze Direct provides these services onsite in dedicated dialysis dens, staffed by specially trained nurses.
Patients receiving MFD in these dialysis dens can expect treatments five days per week, for less than three hours total duration, and do not require costly transportation to offsite dialysis centers.
Various studies have shown benefits to MFD in clinic settings. 8,9 Recovery time in SNF dialysis patients had previously not been studied. Of note, the majority of in-SNF patients treated with MFD by Dialyze Direct are elderly, frail patients with multiple comorbidities.
To answer the question of whether MFD improves post-dialysis recovery times in the SNF population, Dialyze Direct initiated a study of end-stage renal dialysis (ESRD) patients residing in 154 SNFs across twelve states. The total number of patients included in the study criteria was 2,309 patients receiving 108,876 dialysis treatments.
SNF dialysis patients receiving MFD were questioned about recovery to baseline functioning. Results indicated the following: 10
Again, this was despite advanced age, frailty, and multiple complex health conditions. By comparison, DRT within two hours has been reported in only 21-62% of patients receiving conventional dialysis treatment. 11
More frequent dialysis (MFD) offers the possibility of significant ESKD patient quality-of-life enhancements due to improved rehabilitation and long-term (even post-SNF) outcomes.
These important findings are a gateway for further investigation to provide clinical evidence on the benefits of SNF onsite MFD to patient health outcomes and value-based care initiatives.
1 Hellebrand AM, Bellin EY, Kaplan SM. Epidemiology of nursing home dialysis patients- A hidden population. Wiley Online Library. https://onlinelibrary.wiley.com/doi/10.1111/hdi.12943. Published June 16, 2021. Accessed February 21, 2023.
2 Alvarez L, Hu D, Brown D. Intradialytic Symptoms and Recovery Time in Patients on Thrice-Weekly In-Center Hemodialysis: A Cross-sectional Online Survey. Kidney Medicine Journal. https://doi.org/10.1016/j.xkme.2019.10.010. Published December 19, 2019. Accessed February 21, 2023.
3 Bossola M;Di Stasio E;Antocicco M;Silvestri P;Tazza L; Variables associated with time of recovery after hemodialysis. Journal of nephrology. https://pubmed.ncbi.nlm.nih.gov/22941875/. Accessed February 21, 2023.
4 Rayner HC, Zepel L, Fuller DS, et al. Recovery time, quality of life, and mortality in hemodialysis patients: The Dialysis Outcomes and Practice Patterns Study (dopps). American journal of kidney diseases : the official journal of the National Kidney Foundation. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069238/. Published February 14, 2014. Accessed February 21, 2023.
5 Alvarez L, Hu D, Brown D. Intradialytic Symptoms and Recovery Time in Patients on Thrice-Weekly In-Center Hemodialysis: A Cross-sectional Online Survey. Kidney Medicine Journal. https://doi.org/10.1016/j.xkme.2019.10.010. Published December 19, 2019. Accessed February 21, 2023.
6 Alvarez L, Hu D, Brown D. Intradialytic Symptoms and Recovery Time in Patients on Thrice-Weekly In-Center Hemodialysis: A Cross-sectional Online Survey. Kidney Medicine Journal. https://doi.org/10.1016/j.xkme.2019.10.010. Published December 19, 2019. Accessed February 21, 2023.
7 Hellebrand AM, Bellin EY, Kaplan SM. Epidemiology of nursing home dialysis patients- A hidden population. Wiley Online Library. https://onlinelibrary.wiley.com/doi/10.1111/hdi.12943. Published June 16, 2021. Accessed February 21, 2023.
8 More Frequent Dialysis Improves Health of Kidney Patients. National Institutes of Health. https://www.nih.gov/news-events/nih-research-matters/more-frequent-dialysis-improves-health-kidney-patients. Published July 6, 2015. Accessed February 21, 2023.
9 Garg AX, Suri RS, Eggers P. Patients receiving frequent hemodialysis have better health-related quality of life compared to patients receiving conventional hemodialysis. Kidney International. https://doi.org/10.1016/j.kint.2016.10.033. Published January 14, 2017. Accessed February 21, 2023.
10 Hellebrand AM, Kaplan SM, Ledvina JG, Markis WT, Levin NW, Kaufman AM. Post-dialysis recovery time in ESRD patients receiving more frequent hemodialysis in skilled nursing facilities. Hemodialysis International. International Symposium on Home Hemodialysis. https://onlinelibrary.wiley.com/doi/10.1111/hdi.13012. Published April 6, 2022. Accessed February 28, 2023.
11 Hellebrand AM, Kaplan SM, Ledvina JG, Markis WT, Levin NW, Kaufman AM. Post-dialysis recovery time in ESRD patients receiving more frequent hemodialysis in skilled nursing facilities. Hemodialysis International. International Symposium on Home Hemodialysis. https://onlinelibrary.wiley.com/doi/10.1111/hdi.13012. Published April 6, 2022. Accessed February 28, 2023.

Alice Hellebrand, DNP, RN, CNN has been with Dialyze Direct since its inception in 2015 and is responsible for overseeing the design and implementation of patient care delivery, clinical staff education, and clinical quality improvement. She has authored many journal publications and her expertise has been sought as a presenter nationally and internationally at nephrology, dialysis, and skilled nursing conferences. Her continued dedication to the Dialyze Direct model of dialysis care gives her unique insights into this pioneering approach to treatment.


There are many moving parts to consider when providing healthcare services during a natural disaster. Hospitals, nursing homes, and other providers must develop and implement emergency plans for these contingencies. In the case of dialysis, there are several important considerations: availability of dialysis equipment, filtration systems for the water used in dialysis, and the sanitation level of the water itself.
The use of in-home dialysis equipment combined with the more frequent dialysis (MFD) model for providing treatment, lends itself naturally to an adaptable approach to managing dialysis care in disaster situations.
Dialyze Direct utilizes the NxStage system, a highly portable dialysis machine that uses far less water than conventional dialysis. Recently, during Hurricane Ian, we saw how this treatment modality, in combination with world-class staff, resulted in a tremendously positive outcome for onsite skilled nursing facility (SNF) patients enrolled in our care.
Conventional dialysis machines are bulky and require a large filtration system. They cannot be easily moved ahead of a natural disaster or easily relocated in the aftermath of one. Especially notable is the fact that they require large amounts of treated water- something that was not readily available after Hurricane Ian’s landfall.
To successfully dialyze patients with conventional dialysis during a natural disaster like Hurricane Ian, massive tanker trucks of water would be needed. With the NxStage machines, approximately 4-6 bags of pre-mixed dialysate weighing around 25 pounds are required for each treatment. During Hurricane Ian, with an appropriate emergency stock of dialysate bags, it was easy to provide safe water in quantities needed to provide treatment. This was despite boil orders in place after flooding occurred.
In addition, because the NxStage system is only 122 pounds and can be taken apart into two separate components and carried, these machines were portable enough to move to sister dialysis sites away from the storm’s direct path. In fact, in an emergency situation like a hurricane, it is possible to only move the top portion of the machine– weighing in at around 55 pounds– and the dialysate bags. In contrast, the entire filtration system and machine would be necessary with a conventional dialysis machine and weighs substantially more- as much as 300 pounds.
Dialyze Direct offers onsite dialysis in treatment “dens” at partner SNFs. These treatments take place five days per week (pursuant to a physician’s order), for a duration of under three hours. Because of this modality, the potential existed ahead of the hurricane to offer treatments earlier in the day than normally scheduled, in order to accommodate time for transportation to facilities away from the storm’s path.
Additionally, in cases where patients were moved to sister facilities and scheduling had to accommodate more patients, these shorter treatment times meant that it was easier to coordinate scheduling dialysis for an increased patient census.
During Hurricane Ian, Dialyze Direct’s patients saw the immediate benefit of having access to multiple onsite options. Because the SNFs they resided in had sister facilities that also partnered with Dialyze Direct, these residents were able to be relocated, along with the NxStage equipment, to alternative SNFs for treatment.
This process of continuing treatments was seamless, with electronic medical records transferring easily, and staff willingly relocating temporarily to assist patients with their care needs. Where other SNFs may have been forced to relocate some patients to local hospitals for care, further burdening the healthcare system and occupying beds needed for medical emergencies, Dialyze Direct patients were able to avoid hospitalizations, both during and after the disaster.
To deliver dialysis care with the NxStage system and MFD, Dialyze Direct’s nurses and team members are specially trained. During Hurricane Ian, their unique and patient-centered care was especially highlighted, as caregivers mobilized to work both earlier and later than their usual shifts to ensure all patients received their prescribed treatments. Staff were also willing to leave their homes for extended periods to stay with patients at non-local SNFs to offer dialysis until they could be safely transferred back to their original SNFs.
It is this dedication and innovation that is at the heart of what Dialyze Direct does. Our dialysis patients in partner SNFs can expect better recovery times and better quality of life, and as this natural disaster illustrated, continuity of care even in challenging times.
For more information on how to join more than 200 locations in 14 states in bringing the Dialyze Difference to patients, contact David Schneck, Director of Managed Care, at (718) 506-1739, or via email at dschneck@dialyzedirect.com.

Gilda Jones, RN, CNN is a seasoned nephrology nurse who has experience spanning nearly 4 decades, from clinical care to roles as director of nursing. As Vice President of Clinical Services for Dialyze Direct, she provides education to staff and patients, oversees patient outcomes and manages all aspects of the dialysis units for which she is responsible. She enjoys mentoring nursing staff and providing CEU programs to help nephrology nurses excel at dialysis care.

