Stages of Chronic Kidney Disease: What You Need to Know
09/18/2025
Chronic kidney disease (CKD) is a growing health concern, affecting 1 in 7 adults in the United States, nearly 37 million people, according to the Centers for Disease Control and Prevention (CDC). Alarmingly, 90% of those with CKD are unaware they have it until the disease has progressed to more severe stages (National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)).
Often called a “silent disease,” CKD develops gradually, with no noticeable symptoms in the early stages. By the time most people receive a diagnosis, significant kidney damage has already occurred, increasing their risk of kidney failure, heart disease, stroke, and even death.
The kidneys play a vital role in filtering toxins and excess fluids from the blood, regulating blood pressure, producing red blood cells, and maintaining electrolyte balance. When kidney function declines, these essential processes are disrupted, leading to severe health complications. In fact, CKD and heart disease are closely linked, as reduced kidney function increases the risk of cardiovascular problems.
The Five Stages of Chronic Kidney Disease: A Closer Look
The stages of CKD are determined by the glomerular filtration rate (GFR) which is calculated using serum creatinine levels, and is a measure of how well the kidneys filter waste.
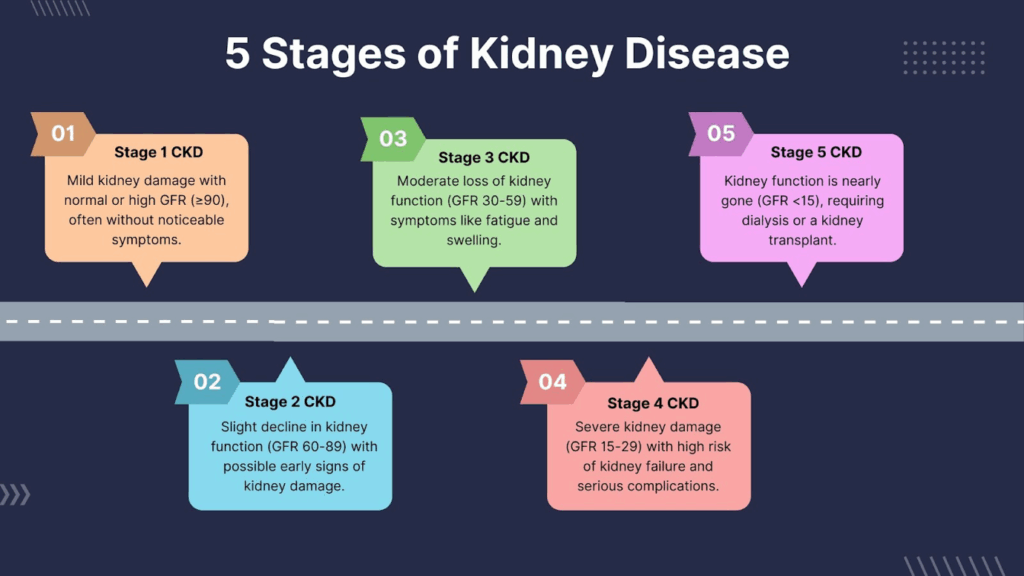
Stage 1 CKD: Kidney Damage with Normal Function
GFR: 90 or above (kidneys function normally but show damage signs).
Possible Signs:
- Protein in urine (albuminuria) – an early indicator of kidney damage.
- Kidney imaging abnormalities can be explored with ultrasound or other imaging studies.
Symptoms: None in most cases; only detected through routine screening.
Fact: At this stage, lifestyle changes and/or other interventions may mitigate further kidney damage.
Management:
Control of risk factors. The detailed management depends on the underlying cause. For example, control of hypertension or diabetes can help. Appropriate dietary interventions (lowering dietary sodium, sweets or protein) may also be appropriate. Regular kidney function monitoring should be initiated.
Stage 2 CKD: Mild Kidney Dysfunction
GFR: 60-89
Symptoms:
Mild changes in urine output or urine character (e.g., foamy urine may occur with more significant urinary protein losses), or mild fluid retention causing lower extremity swelling (edema) may also be present.
Fact: People with high blood pressure or uncontrolled diabetes are at higher risk of CKD progression.
Management:
In addition to hypertension and diabetes management, regular kidney function tests must be carefully tracked. Avoid NSAIDs (like ibuprofen), which can accelerate kidney damage.
Stage 3 CKD: Moderate Loss of Kidney Function
GFR: 30-59
Symptoms:
Fatigue and weakness can manifest due to the development of advanced CKD-related anemia. More extensive swelling of the feet (and sometimes hands and face) may be associated with more fluid retention.
Complications of CKD: Increased risk of heart and vascular disease. At this stage of kidney disease, abnormalities of calcium, phosphorus, and bone metabolism begin to manifest.
Fact: At Stage 3, 1 in 3 people with CKD may develop end-stage kidney disease (ESKD) without proper management.
Management:
Medications to control blood pressure, blood sugar, and phosphorus levels may be indicated. Reduced protein intake may also be indicated in some circumstances to lessen the burden on the kidneys.
Stage 4 CKD: Severe Kidney Dysfunction
GFR: 15-29
Symptoms:
- Severe swelling may now include fluid in the lungs, leading to difficulty breathing.
- Nausea and loss of appetite due to toxin buildup may become prominent.
- Abnormalities in red blood cells (anemia) may also become prominent.
- Itchy, dry skin and changes in skin color may develop.
- Risk of Kidney Failure: High, with dialysis or a kidney transplant potentially imminent.
Fact: More than 50% of people with Stage 4 CKD will develop kidney failure within five years.
Management:
Rule out any superimposed kidney obstruction with imaging studies, even if it was ruled out at an earlier stage of kidney disease. Begin discussing dialysis and/or kidney transplant options with your kidney specialist. Carefully monitor and manage anemia and electrolyte imbalances.
Stage 5 CKD: End-Stage Kidney Disease (ESKD)
GFR: Below 15 (kidney function is at a critically low level).
Symptoms:
Severe fatigue, weakness, confusion due to toxin buildup and anemia. Shortness of breath due to fluid in the lungs. Significant swelling (legs, around the eyes, and abdomen).
Treatment Options:
Dialysis (hemodialysis or peritoneal dialysis) to filter toxins from the blood. Kidney transplantation (if appropriate) offers the best long-term survival outcome. Home dialysis is an option for many patients, offering flexibility, improved quality of life and superior medical outcomes. Learn more about home dialysis here.
Understanding Albuminuria Stages in Chronic Kidney Disease
Albuminuria is a key indicator of kidney disease, referring to the presence of albumin (a type of protein) in the urine. Healthy kidneys typically prevent normal blood protein from leaking into the urine, but when kidney function declines, significant protein in the urine signals kidney damage. Measuring albuminuria helps assess the severity of chronic kidney disease (CKD) and predict the risk of progression to kidney failure.
Albuminuria Stages and Their Significance
The National Kidney Foundation classifies albuminuria into three stages based on the albumin-to-creatinine ratio (ACR) in milligrams (mg) albumin per gram (g) creatinine):
A1 (Normal to Mild Albuminuria)
ACR: Less than 30 mg/g
This level is considered normal or mildly increased. It typically does not indicate significant kidney damage. However, people with diabetes, high blood pressure, or other CKD risk factors should monitor their kidney health closely.
A2 (Moderate Albuminuria, formerly known as Microalbuminuria)
ACR: 30–300 mg/g
A moderate increase in albumin levels suggests early kidney damage. At this stage, CKD may still be reversible with lifestyle changes and medication to control blood pressure, diabetes, and other contributing factors.
A3 (Severe Albuminuria, formerly known as Macroalbuminuria)
ACR: More than 300 mg/g
A high level of albumin in the urine indicates significant kidney damage. This stage is associated with a higher risk of CKD progression, cardiovascular disease, and end-stage kidney disease (ESKD), requiring dialysis or a kidney transplant.
Why Albuminuria Matters
- Early Detection: Even mild albuminuria can signal kidney dysfunction before a decline in the glomerular filtration rate (GFR) is detected.
- Risk Assessment: Higher albuminuria levels correlate with an increased risk of CKD progression, heart disease, and mortality.
- Treatment Guidance: Controlling albuminuria through certain medication (like ACE inhibitors or ARBs), diet, and lifestyle modifications can slow CKD progression and reduce complications.
Testing for Albuminuria
A simple urine albumin-to-creatinine ratio (uACR) test can detect albuminuria. The National Kidney Foundation recommends regular testing for individuals at high risk, including those with diabetes, high blood pressure, or a family history of kidney disease.
Understanding albuminuria stages can help people with CKD take proactive steps to preserve kidney function and prevent the progression of kidney failure.
Causes and Risk Factors of CKD
CKD can develop due to various underlying conditions, with diabetes and high blood pressure being the leading causes.
- Diabetes and Kidney Disease: High blood sugar damages kidney blood vessels, leading to a gradual loss of kidney function.
- High Blood Pressure (Hypertension): Increased pressure on kidney arteries causes long-term damage.
- Polycystic Kidney Disease (PKD): A genetic disorder where fluid-filled cysts impair kidney function.
- Acute Kidney Injury (AKI): Sudden kidney failure from an acute medical condition that injures the kidneys. Examples include but are not limited to infections, shock, or medications. AKI is often reversible, but not always reversible.
- Cardiovascular Disease: Heart disease and kidney disease are closely linked, as kidney function loss can increase the risk of heart failure.
- Family History of Kidney Disease: Increases risk of kidney disease significantly.
Who Is at Risk?
- Individuals with diabetes or hypertension.
- People with a family history of kidney disease.
- Those who are obese or smoke.
African American, Hispanic, Asian, and Native American populations have a higher genetic predisposition, but proteinuria can also occur in individuals of any heritage.
Early Detection & Prevention Strategies
How to Detect CKD Early
- Blood Tests: Measure serum creatinine levels and calculate GFR.
- Urine Tests: Check for albuminuria (protein in urine).
- Blood Pressure Monitoring: High blood pressure is both a cause and consequence of CKD.
How to Prevent CKD Progression
- Follow a Kidney-Friendly Diet: Limit salt, processed foods, red meat, and phosphorus-rich foods.
- Stay Hydrated: Aim for at least 2-3 liters of water daily (unless advised otherwise by a doctor).
- Manage Blood Sugar & Blood Pressure: Keep HbA1c below 7% (for diabetics) and BP below 130/80 mmHg.
- Exercise Regularly: Aim for 150 minutes of moderate exercise per week.
- Avoid Nephrotoxic Medications: Limit use of NSAIDs (like ibuprofen).
- Quit Smoking & Reduce Alcohol Intake: Both can worsen kidney function.
Support for Patients with Advanced CKD
At Dialyze Direct, we understand how overwhelming a CKD diagnosis can feel. That’s why we provide personalized, more frequent home hemodialysis treatments inside SNFs or within a patient’s home. Our approach is designed to be gentler on the body, easier to fit into daily life, and to provide superior medical outcomes.
If you’re a patient, caregiver, or healthcare provider, contact Dialyze Direct today to learn how we can help support better outcomes for people living with advanced kidney disease.
Phone: (732) 732-0052
Web Address: https://www.dialyzedirect.com/contact/
FAQs
Life expectancy varies and is influenced by the underlying medical conditions. However, with proper management, many people with stage 3 CKD can live for decades without progressing to kidney failure.
The five stages of CKD range from mild kidney damage (Stage 1) to end-stage kidney disease (Stage 5), classified by glomerular filtration rate (GFR) levels.
It is recommended to see a nephrologist by Stage 3 CKD to monitor kidney function and slow disease progression. Often a nephrologist is seen at an even earlier stage of kidney disease.
While CKD is generally not reversible, lifestyle changes, medication, and proper disease management can slow or halt its progression.
Information contained in this blog is for informational or educational purposes only and does not substitute professional medical advice or consultations with healthcare professionals. The content is not intended to be comprehensive or exhaustive, and it does not apply to any specific individual’s medical condition. Always refer to the personalized information given to you by your doctor, or contact us directly.

Dr. Allen Kaufman is the Chief Medical Officer and Senior VP for Clinical & Scientific Affairs at Dialyze Direct, with over four decades of experience in Nephrology. He began his career in 1980 and has held leadership roles including Chief of Nephrology & Hypertension at Beth Israel Medical Center (1998–2004), Chief of Dialysis at the Bronx VA Medical Center (1982–1990), and Chief of the Yorkville Dialysis Unit at Beth Israel and the Renal Research Institute (1990–2000). Dr. Kaufman has authored over 100 scientific publications and served as Principal or Co-Investigator on numerous NIH-funded research studies. A Fellow of the American College of Physicians, he is board-certified in Nephrology and Internal Medicine. He earned his medical degree from the University of Rochester and completed training at the Hospital of the University of Pennsylvania and Mount Sinai in New York. Dr. Kaufman is widely recognized with multiple “Best Doctor” and “Patients’ Choice” awards.